As you may recall from my article, How the government murdered tens of thousands of grandmas in 2020, Jack and I noted that the ventilation procedure, without any treatment for inflammation and coagulation, ended up making the cytokine storm (the inflammatory response in the body) worse, killing tens of thousands, if not hundreds of thousands of people.
See: /@thepholosopher/how-the-government-murdered-tens
We noted in the article that the focus on ventilators dropped out of media headlines once this information started to emerge.
But few people have heard about what has changed in hospitals since early ventilation protocols to adjust for the risk of inflammation and ventilator-induced pneumonia.
On ventilator-induced pneumonia, see:
Ventilator-Associated Pneumonia: Diagnosis, Treatment, and Prevention
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1592694/
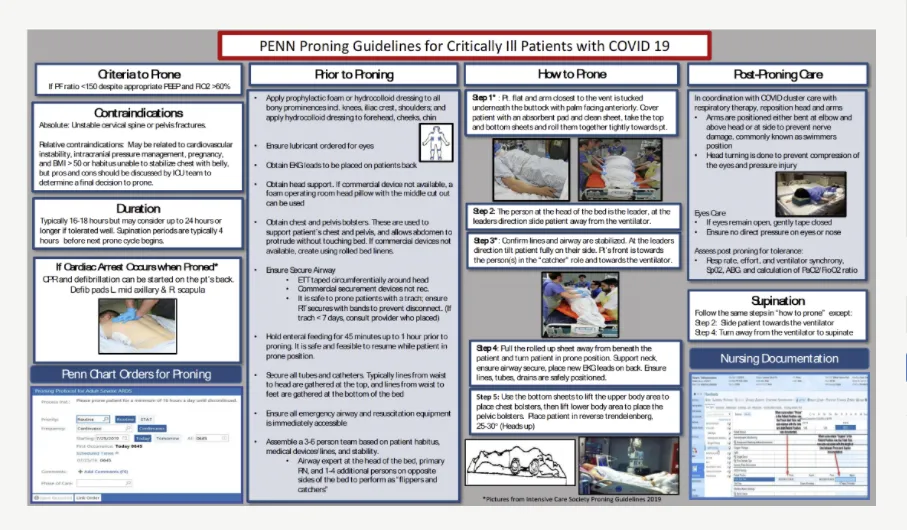
The specific change that took place was a switch to “proning,” that is, instead of having the patient lie on their back, they would have their body turned to face the bed.
The University of Pennsylvania’s Medical blog notes this change in practice, emphasizing that while at first not widespread, it has now become more than anecdotal.
See: Proning During COVID-19
https://www.pennmedicine.org/updates/blogs/penn-physician-blog/2020/may/proning-during-covid19
Penn researchers stated that proning is critical because:
“Physical position affects the distribution and volume of air in the lungs, and can have direct effects on the expansion or collapse of the delicate alveoli that permit the exchange of oxygen and carbon dioxide in the blood. It has long been known that the supine position—lying on the back—can be detrimental to underlying pulmonary function, particularly for patients on mechanical ventilation. Like many in-hospital procedures, mechanical ventilation is typically administered in the supine position.”
...Gravity complicates things by pushing blood downward toward the poorly oxygenated alveoli in the posterior lung, creating a ventilation/perfusion mismatch. This mismatch is thought to drive rapid deterioration of patients with ARDS and other conditions that compromise breathing.”
The possible benefits noted are:
The evidence for support of this change has been noted in the New England Journal of Medicine published paper,
Improving Prone Positioning for Severe Acute Respiratory Distress Syndrome during the COVID-19 Pandemic An Implementation-Mapping Approach
https://www.atsjournals.org/doi/pdf/10.1513/AnnalsATS.202005-571OC
That all said, it’s important to recognize just how much one small change can radically improve health outcomes for patients.
Which is precisely why thinking through outpatient treatment protocols is essential to reducing hospitalizations and deaths.
For more on outpatient protocols, see:
I-MASK+ Prevention & Early Outpatient Treatment Protocol for COVID-19
https://covid19criticalcare.com/covid-19-protocols/i-mask-plus-protocol/
and
Pathophysiological Basis and Rationale for Early Outpatient Treatment of SARS-CoV-2 (COVID-19) Infection
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7410805/
#coronavirus #covid #covid19 #corona #sars2 #sars1 #ventilator #ventilators #ventilation #venting #vaccine #vaccines #vaccination
